Introduction
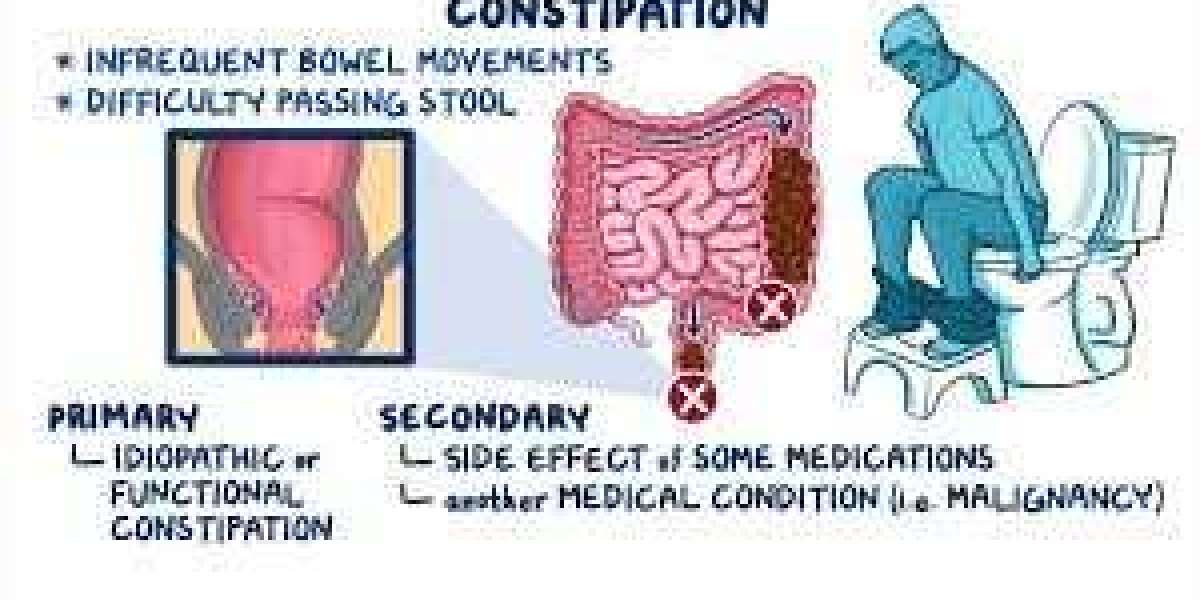
Constipation is a common digestive issue affecting millions of people worldwide. While occasional difficulty in passing stools is normal, persistent constipation can indicate an underlying problem. There are two main Types of Constipation: acute and chronic. Understanding the differences between them can help individuals seek the right treatment and prevent complications. In this blog, we will explore the causes, symptoms, risk factors, complications, and treatments of both acute and chronic constipation.
What Is Acute Constipation?
Acute constipation is a sudden and temporary inability to pass stools. It can last from a few days to a couple of weeks and often resolves with minor lifestyle changes or medical interventions.
Causes of Acute Constipation
Dietary changes – A sudden decrease in fiber or fluid intake can slow bowel movements.
Dehydration – Lack of adequate water intake hardens stools, making them difficult to pass.
Medication side effects – Painkillers, antacids, iron supplements, and antidepressants can cause short-term constipation.
Stress and anxiety – Sudden emotional distress can impact digestive function.
Post-surgical effects – After surgery, anesthesia and pain medications can slow bowel movements.
Travel-related changes – Altered schedules, diet changes, and reduced activity levels may contribute.
Symptoms of Acute Constipation
Infrequent bowel movements (less than three times a week)
Straining during bowel movements
Hard or lumpy stools
Abdominal discomfort or bloating
Temporary loss of appetite
Treatment for Acute Constipation
Increase fiber intake – Whole grains, fruits, and vegetables help soften stools.
Hydrate adequately – Drinking at least 8 glasses of water daily prevents stool hardening.
Exercise regularly – Physical activity stimulates bowel movements.
Use mild laxatives if necessary – Short-term use of laxatives or stool softeners can provide relief.
Avoid holding stools – Ignoring the urge to defecate worsens constipation.
What Is Chronic Constipation?
Chronic constipation is a long-term condition characterized by persistent difficulty in passing stools for weeks or even months. It often requires medical attention and lifestyle modifications for management.
Causes of Chronic Constipation
Low-fiber diet – Consistently consuming low-fiber foods can result in slow bowel movements.
Inadequate fluid intake – Insufficient hydration leads to hardened stools.
Sedentary lifestyle – Lack of physical activity weakens bowel motility.
Chronic medical conditions – Hypothyroidism, diabetes, Parkinson’s disease, and irritable bowel syndrome (IBS) are associated with constipation.
Neurological disorders – Spinal cord injuries or nerve-related conditions can impact bowel function.
Pelvic floor dysfunction – Weakness in the muscles responsible for bowel movements can lead to prolonged constipation.
Long-term medication use – Certain medications, such as opioids and anticholinergics, may cause ongoing constipation.
Symptoms of Chronic Constipation
Infrequent bowel movements lasting several weeks or months
Difficulty or straining while passing stools
Sensation of incomplete evacuation
Hard, dry, or small stools
Chronic bloating or abdominal discomfort
Dependence on laxatives for regular bowel movements
Complications of Chronic Constipation
If left untreated, chronic constipation can lead to severe health issues, such as:
Hemorrhoids – Straining can cause swollen blood vessels in the rectum.
Anal fissures – Hard stools can create small tears in the anal lining.
Fecal impaction – Hardened stools may obstruct the bowel, requiring medical intervention.
Rectal prolapse – Excessive straining can cause part of the rectum to protrude.
Treatment for Chronic Constipation
High-fiber diet – Incorporating whole grains, legumes, and fresh fruits aids digestion.
Hydration – Drinking enough water softens stools and facilitates bowel movements.
Regular physical activity – Walking, yoga, and abdominal exercises stimulate the intestines.
Scheduled bowel habits – Establishing a routine can improve bowel regularity.
Probiotics – Beneficial bacteria support gut health and digestion.
Medical treatment – Prescription medications, biofeedback therapy, or surgery may be necessary for severe cases.
Key Differences Between Acute and Chronic Constipation
| Factor | Acute Constipation | Chronic Constipation |
|---|---|---|
| Duration | Temporary (a few days to weeks) | Persistent (weeks to months or longer) |
| Causes | Diet changes, dehydration, stress, medications | Low-fiber diet, medical conditions, neurological disorders |
| Symptoms | Hard stools, bloating, temporary discomfort | Frequent difficulty in passing stools, long-term discomfort |
| Complications | Usually none or mild | Hemorrhoids, anal fissures, fecal impaction, rectal prolapse |
| Treatment | Diet adjustments, hydration, mild laxatives | Long-term dietary changes, medical intervention, physical therapy |
When to Seek Medical Attention
While occasional constipation is normal, you should consult a doctor if you experience:
Constipation lasting more than three weeks despite lifestyle changes
Severe pain or blood in stools
Unexplained weight loss
Persistent bloating or vomiting
Inability to pass gas or stools for several days
Prevention Tips for Healthy Bowel Movements
Eat a fiber-rich diet – Aim for at least 25-30 grams of fiber daily.
Stay hydrated – Drink plenty of water throughout the day.
Exercise regularly – Physical activity promotes bowel motility.
Establish a bathroom routine – Train your body to follow a consistent schedule.
Manage stress – Practice relaxation techniques like meditation and deep breathing.
Conclusion
Understanding the differences between acute and chronic constipation is crucial for effective prevention and management. While acute constipation is often short-lived and resolves with simple lifestyle changes, chronic constipation requires ongoing care and medical attention. By maintaining a healthy diet, staying active, and addressing underlying medical conditions, you can promote optimal digestive health and prevent long-term complications.